At URGO Medical, we are here to heal people. It is our mission to support healthcare professionals and make a difference in the lives of their patients.
We aim to work in partnership with healthcare professionals to move from managing wounds to healing wounds to help improve patient outcomes and reduce healing time.
Jenny’s Story
Jenny sustained an injury after falling off her bike. The wound then became chronic and long-lasting which caused some frustration due to its delayed healing. Hear Jenny’s full healing journey and how she managed to return enjoying the activities she loves – riding her bike and being at the beautiful beach.
Rob’s Story
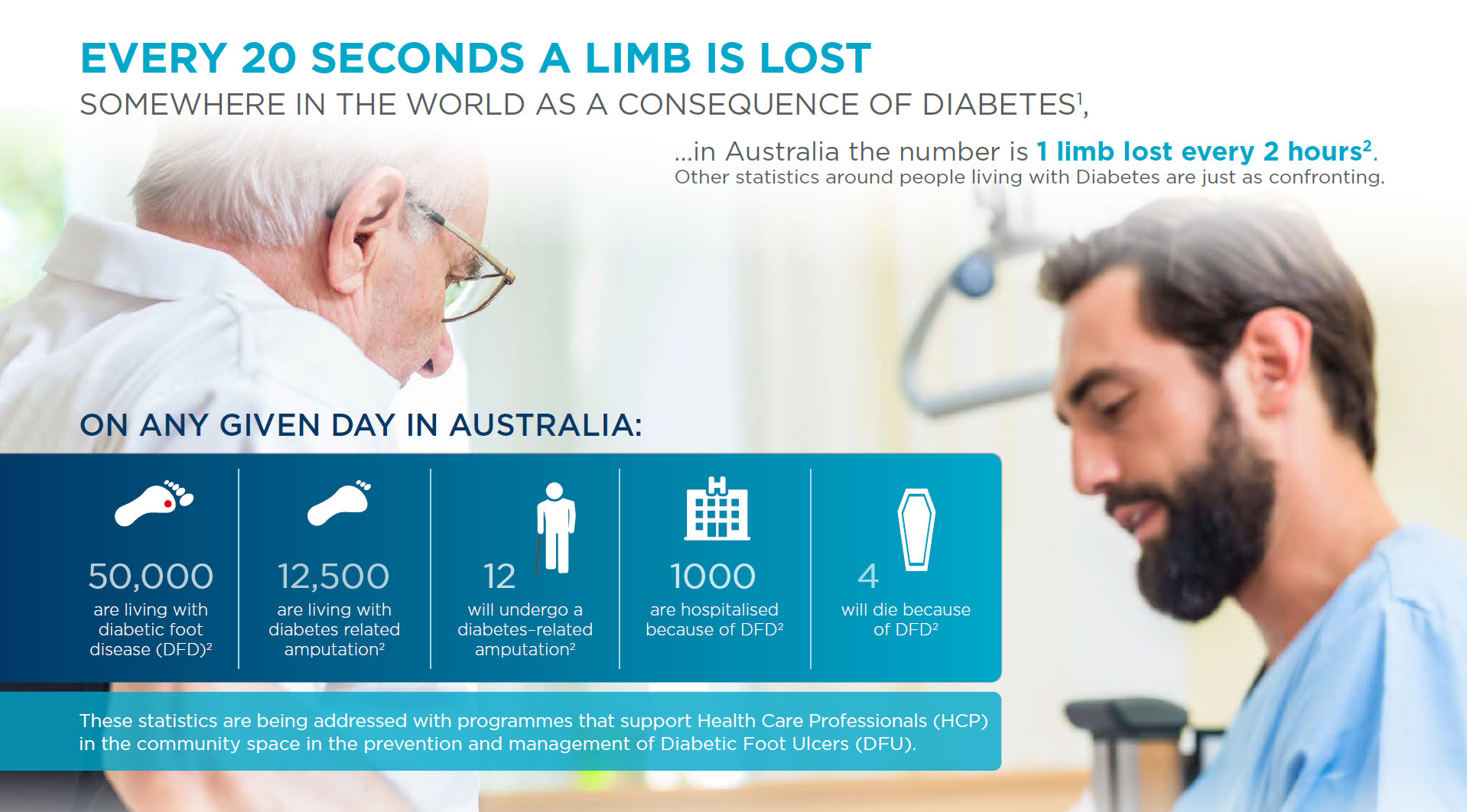
After Rob sustained a diabetes-related foot ulcer whilst travelling overseas with his wife, he struggled to find relief from his chronic wound. Tune in to listen to Rob’s journey to healing as he navigates the complexities of having diabetes and finally achieving relief.