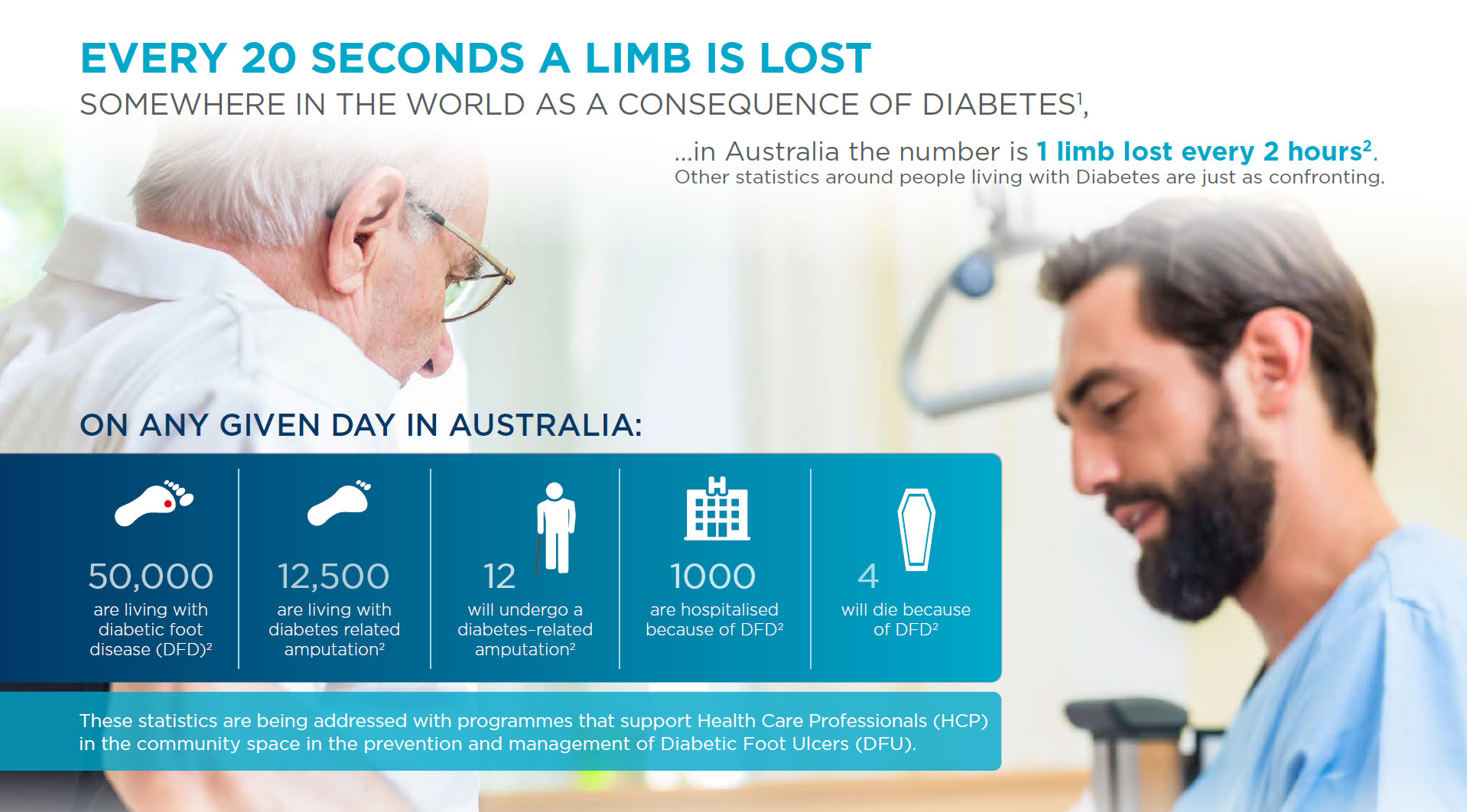
Diabetic foot ulcers (DFUs)are one of the major complications of diabetes. Between 19 and 34% of all diabetics will develop a foot ulcer at some point in their lives3 DFUs can lead to complications such as an infection requiring hospitalisation, or in the worst cases, amputation. After amputation, patient life expectancy does not exceed 5 years in almost 70% of cases4.
PREVENTION OF DFUs
The prevention of DFUs requires a partnership of those people living with Diabetes and their HCP. This partnership should be underpinned with daily foot checks undertaken by the patient, reinforced by regularly scheduled visits to their HCP for a more detailed check that should, at a minimum include a check for Loss of Protective Sensation (LOPS) due to neuropathy and Peripheral Artery Disease (PAD). Both of these are major risk factors in the development of DFUs.
To assist in the rating of patient’s risk of developing a DFU URGO Medical Australia have provided Fact Sheets for both General Practitioners and their patients, now available in Medical Director and Best Practice, on diagnosis.
This Fact Sheet also provides GPs with a link to the Australian Save Feet/Save Lives website where you can find more information on the prevention of DFUs. A non-HCP version of the site is also available for patients to learn more about Diabetes and preventative care of their feet.
MANAGEMENT OF DFUs
With the best of efforts, a large number of DFUs still occur. This is when closing wounds earlier reduces the risk of amputation 5,6. There are steps that can be taken by front line healthcare practitioners to better managing a DFU.
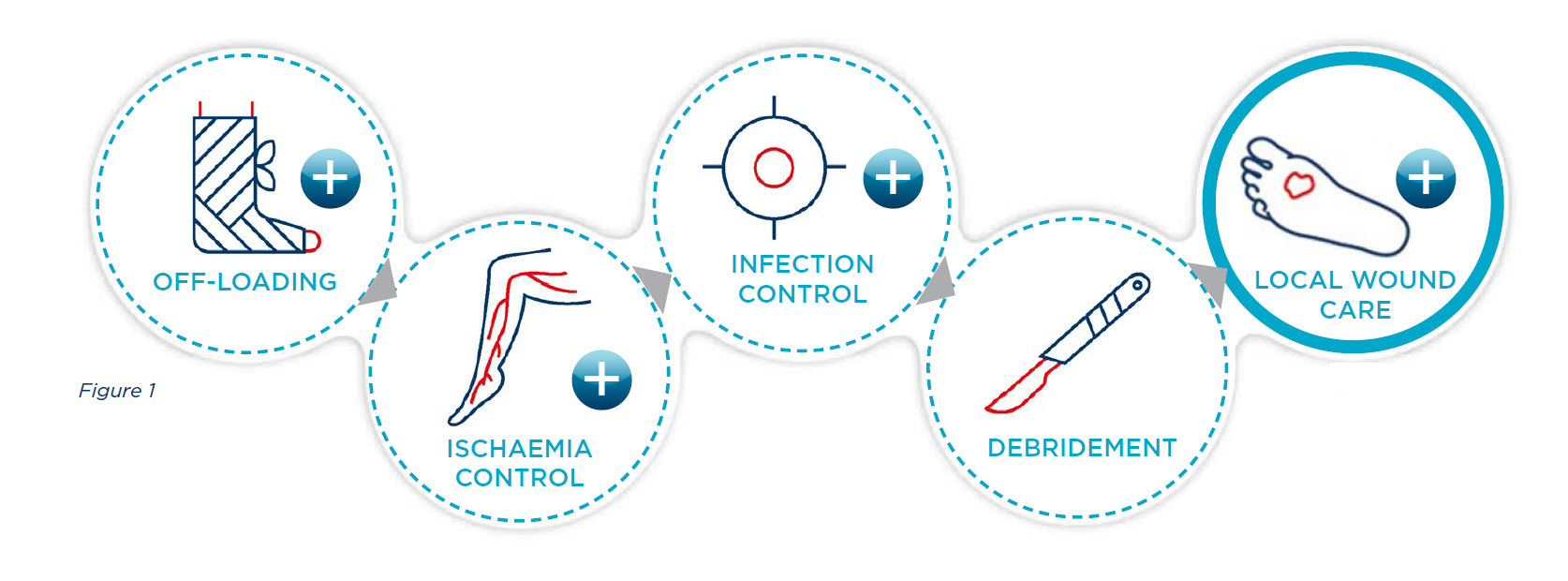
UNDERSTAND THE STANDARD OF CARE FOR DIABETIC FOOT ULCERATION. DFU treatment is complex and requires a multidisciplinary approach. This is the recommended standard of care that needs to be put in place by a multidisciplinary team in a specialised setting5,6 (also see figure 1)
REFERENCES
- Whiting, D. R., Guariguata, L., Weil, C., and Shaw, J. 2011. “IDF Diabetes Atlas: Global Estimates of the Prevalence of Diabetes for 2011 and 2030.” Diabetes Res. Clin. Pract. 94 (3): 311-21.
- Van Netten JJ, Lazzarini PA, Fitridge R, Kinnear E, Griffiths I, Malone M, Perrin BM, Prentice J, Sethi S, Wraight PR. Australian diabetes-related foot disease strategy 2018-2022: The first step towards ending avoidable amputations within a generation. Brisbane: Diabetic Foot Australia, Wound Management CRC; 2017.
- Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med 2017; 376: 2367-75
- Walsh JW, Hoffstad OJ, Sullivan MO, Margolis DJ. Association of diabetic foot ulcer and death in a population-based cohort from the United Kingdom. Diabet Med 2016; 33:1493–98.
- Frykberg RG. Diabetic foot ulcers: pathogenesis and management. Am Fam Physician 2002; 66(9): 1655-62.
- Vuorisalo S, Venermo M, Lepantälo M. Treatment of diabetic foot ulcers. J Cardiovasc Surg 2009; 50(3): 275-91.


